At a recent press conference organized by Cancerinformation.com.hk and Hong Kong Health Care Alliance, a leading clinical oncologist and two advanced practice nutrition experts tackled the issue of cancer-related malnutrition and discussed the impact and management of oral mucositis, a common and debilitating complication of anticancer treatments.
The oral cavity is highly susceptible to the direct and indirect toxic effects of cancer treatments, such as CT and RT, particularly in patients with head and neck cancer (HNC). In particular, the oral cavity is especially susceptible to cancer treatment-related toxicity because of the rapid rate of cell turnover in the mucosal lining.
Oral mucositis is the most debilitating treatment-related toxicity of HNC. According to the European Oncology Nursing Society, the risk of developing oral mucositis following many standard CT regimens for patients with HNC is approximately 40%, while all patients administered high-dose RT for HNC are expected to experience mucositis. Furthermore, patients receiving head and neck RT alone, or as chemoradiotherapy (CRT), are more likely to develop severe oral mucositis than those receiving CT alone.
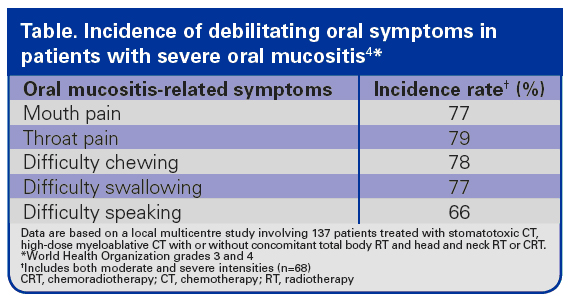
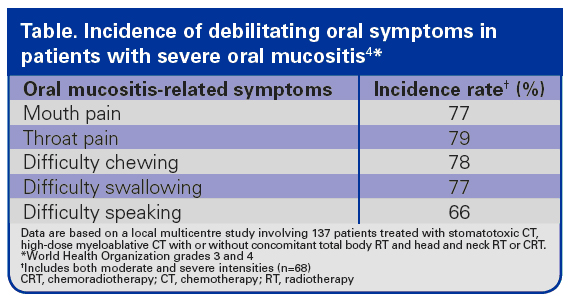
Many patients with severe oral mucositis suffer from a multitude of coexisting moderate or severe oral symptoms (Table) that cause profound pain, oral functional incapability, sleep disturbances, depression and reduced QoL. Patients who have been treated for HNC may experience weight loss and nutritional deficiencies as difficulty chewing and swallowing, as well as taste disturbances and pain, may limit their nutritional intake. Patients with HNC and treatment-related oral mucositis are significantly more likely to have weight loss of more than 5% compared with patients without oral mucositis (60% vs 17%; p<0.001); mean weight loss was 3kg for patients with any grade of oral mucositis and 4kg for patients with 3 or 4 oral mucositis and 4kg for patients with grade 3 or 4 oral mucositis. Moreover, oral mucositis is associated with an incremental cost of US$1,700-US$6,000 per patients, depending on the grade.
Treatment-related severe oral mucositis can also lead to dose reduction or a temporary interruption or delay of treatment. The average duration of hospitalization is significantly longer during CT cycles for patients who have developed CT-related oral or gastrointestinal mucositis, and CT dose reduction is twice as common in patients who develop oral mucositis than those who do not. Thus, oral mucositis can be a dose-limiting side effect of CT with direct effects on treatment outcomes.
Severe oral mucositis-related pain can significantly compromise nutritional intake. Furthermore, treatment-related changes in taste can further decrease patient appetite, potentially leading to malnutrition. Immunonutrition supplements may prevent severe oral mucositis, reduce the risk of postoperative infection and shorten the length of hospital stay for patients with cancer. Oral supplementation with a specialized formula containing L-arginine, omega-3 fatty acids, ribonucleic acids and a mix of antioxidants, vitamins and micronutrients (immunonutrition) has been shown to reduce inflammatory markers in patients with stage III or IV HNC treated with concomitant CRT. Furthermore, the incidence of severe acute mucositis in patients who received immunonutrition was 16%, whereas earlier studies of patients treated with RT alone or CRT reported a prevalence of severe acute mucositis of 45% (Figure).
Effective management of the symptoms of oral mucositis may improve nutritional intake and QoL. The use of saline mouth rinses, ice chips and topical mouth rinses containing a local anaesthetic can control oral mucositis-associated pain. Sipping water, using artificial saliva or non-medicated mouth rinses, and chewing sugarless gum can alleviate mouth dryness, thereby reducing the risk of oral inflammation and infection. Additionally, a standardized oral care protocol, including brushing with a soft toothbrush, flossing and gargling with saline or sodium bicarbonate rinse, is essential to minimize microbial colonization of lesions and may help to reduce the risk of exacerbating oral mucositis.
Oral mucositis is a clinically important and potentially dose-limiting complication of anticancer therapy. Severe mucositis lesions can cause significant pain, interfere with nutritional intake and may necessitate interruption or delay of a patient’s treatment. Immunonutrition supplements containing arginine, omega-3 fatty acids and ribonucleic acids may prevent severe oral mucositis and improve patient outcomes. Applying effective management strategies for patients who do develop oral mucositis may also enhance nutritional intake, reduce the risk of exacerbating any symptoms and improve patient QoL.
